Background: Rapid I-131 turnover Graves’ disease patients have low cure rate. We aimed to compare cure percentage at 12 months among 3 treatment doses of I-131 with or without lithium carbonate (LiCO3) in rapid turnover Graves’ disease patients.
Methods: Sixty Graves’ disease patients referred for radioactive iodine treatment were randomised into three arms of treatment: Group A, 3.7 MBq I-131/g thyroid plus 600 mg/day LiCO3, Group B, 5.55 MBq I-131/g plus 600 mg/day LiCO3, and Group C, 7.4 MBq I-131/g without LiCO3. Data were collected at baseline, 3, 6, 9, and 12 months. The primary endpoint were cure rates (percentage of euthyroid or hypothyroid) at 12 months. Pairwise comparisons were made across 3 groups using an equality of proportions test. The secondary endpoint, the odds of cure over the total follow-up for group B and C versus group A, was analyzed using generalized estimating equation (GEE). Side effects of I-131 and LiCO3 treatment were evaluated at 1 to 2 weeks after treatment.
Results: The cure rate at 12 months was 45% (9/20) for group A, 60% (12/20) for group B and 80% (16/20) for group C. The mean difference in proportion cured at 12 months between group C and group A was 35 (7.0 to 66.8)%; P-value = .02. There was a statistically significant difference between cure rates over all follow-up of group C and A after adjustment for sex (adjusted OR = 3.09; 95%CI = 1.32–7.20; P-value = .009), but no significant difference was found between group B and A or C and B in the primary and/or secondary efficacy endpoints. Side effects from the treatment were found in 12% (7/60); 2 in group A, 4 in group B, and 1 in group C. Four of these were likely due to LiCO3 side effects.
Conclusions: Treatment of rapid turnover Graves’ disease patients with high dose I-131 (7.4 MBq/g) provides significantly higher cure rates at 12 months, and 3 times odds of cure than 3.7 MBq/g I-131 plus LiCO3 with lesser side effects. We thus recommend 7.4 MBq I-131/g for treatment in these patients.
1 Introduction
Graves’ disease in the most common cause of hyperthyroidism.[1] Among patients with Graves’ disease, about 15% have a rapid I-131 turnover (4/24 hours uptake ratio > 1),[2] which is associated with I-131 treatment failure of approximately 50% using a standard I-131 treatment dose of 3.70–5.55 MBq/g (100–150 microCi/g) of thyroid tissue.[3] Studies have shown that lithium carbonate (LiCO3) increases intrathyroidal iodine content by inhibiting the discharge of I-131 from the thyroid gland.[4] This results in increased I-131 resident time in the thyroid and thus may lead to increased cure rates when LiCO3 is used together with I-131. However, the role of using LiCO3 together with I-131 to enhance the cure rate in hyperthyroidism is still controversial and studies have shown conflicting results.[5–8] Although LiCO3 decreases rapid turnover in Graves’ disease patients,[9,10] the cure rate after a single dose of I-131 treatment with this regimen has not been extensively studied. Until now, there is no consensus for the optimal regimen to treat Graves’ disease with rapid turnover.
The purpose of this study was to compare the effectiveness of treatment among standard dose 3.7 MBq/g (100 microCi/g) I-131 plus LiCO3, high dose 5.55 MBq/g (150 microCi/g) I-131 plus LiCO3 and high dose 7.4 MBq/g (200 microCi/g) I-131 in rapid turnover Graves’ disease patients.
2 Material and methods
2.1 Study design
This was a parallel, 3-arm randomized trial, which the Graves’ disease patients with rapid I-131 turnover (4 hours uptake/24 hours uptake > 1) were randomised into three treatment groups by block of 3 with allocation concealment using envelopes in a box. After written informed consent was obtained, a nurse not involved in the study was assigned to blindly pick one envelope containing the sequence of treatment assignment, for example, A–B–C or A–C–B, etc. After knowing the sequence of treatment group, the nurse then informed the physician who treated the patient of the sequence of treatment for every 3 patients. Treatment in each group was assigned as follows: Group A, 3.7 MBq/g thyroid (100 microCi/g) I-131 plus 600 mg/day LiCO3 for 7 days after I-131 treatment; group B, 5.55 MBq/g (150 microCi/g) I-131 plus 600 mg/day LiCO3 for 7 days after I-131 treatment; and group C, high dose 7.4 MBq/g (200 microCi/g) without LiCO3.
This study was approved by the institutional review board of the Faculty of Medicine, Chulalongkorn University (COA No. 253/2015). The study was registered in the Thai Clinical Trials Registry website before enrollment of the first patient at www.clinicaltrials.in.th (TCTR20151023001).
2.2 Participants
Sixty Graves’ disease patients with rapid I-131 turnover who were referred to the Nuclear Medicine division, Department of Radiology, King Chulalongkorn Memorial Hospital for radioactive iodine treatment between April 2015 and June 2016 were enrolled. The inclusion criteria were thyroid gland weight >50 grams and age >18 years. The exclusion criteria were previous treatment with I-131 or thyroid surgery, pregnancy or lactation.
2.3 Procedure
Thyroid uptake was performed 4 and 24 hours after 25 μCi I-131 oral administration using an Atomlab 950 thyroid uptake probe (Biodex, NY) counting at the thyroid for 60 seconds with photopeak of 364 keV ± 15% window. Thyroid scan was performed for 15–30 minutes, following intravenous injection of 74 to 185 MBq (2–5 mCi) of Tc-99m pertechnetate after finishing the thyroid uptake procedure on the second day. The image was acquired in the anterior view with a 256x256 matrix, LEHR collimator, photopeak 140 keV ± 20% window using an e.cam SPECT camera (Siemens, Erlangen, Germany). Thyroid gland size in grams was calculated using the Allen and Goodwin formula.[11] Actual dosage of I-131 treatment for each study group as stated above was then calculated using the formula: [12,13]
2.4 Outcome measures and statistical analysis
The cure rate (percentage of patients with euthyroid or hypothyroid status) in each group was evaluated at 3, 6, 9, and 12 months by monitoring thyroid gland size and thyroid function tests (FT3, FT4 and TSH). A repeat dose of I-131 treatment was allowed during the follow up period if the attending physician thought that there was no, or minimal response to I-131 treatment. In these patients, we defined their status as “not cured” throughout the remaining follow-up.
Side effects of I-131 and LiCO3 treatment were evaluated by telephone interview, 1–2 weeks after treatment. Any new symptoms occurring after I-131 and/or LiCO3 treatment were recorded and defined as side effects. Other factors including age, sex, family history of hyperthyroidism, the duration of disease prior to radioactive iodine treatment, type and duration of treatment by antithyroid drug (ATD), thyroid gland size by thyroid scan were recorded in the study database.
Statistical analyses were performed using Stata 15.1 (Statacorp, College Station, TX).[14] Statistically significance was set at P-values <.05. Sample size calculations were based on an improvement in the cure rates at 12 months in groups B or C versus group A. We assumed the cure rate in group A would be 45%. Enrolling 20 patients per group would allow us to assess a doubling of the cure rate to 90% in groups B or C at 80% power and a 2-sided significance level of 5%. Baseline categorical characteristics were reported as N (%) and continuous covariates were described as median (interquartile range, IQR). The primary endpoint was the proportion of patients cured at 12 months; pairwise comparisons of proportions cured were made across the 3 groups using an equality of proportions test, to calculate the difference in the cured proportions (95%CI). The primary analysis was intention to treat (ITT), where patients were analyzed according to their randomised arm, and missing data were imputed as failure (i.e., not cured). A secondary analysis excluded missing data.
We also compared the odds of cure over the total follow-up as a secondary endpoint for group B and C versus group A as a reference group, using a generalized estimating equation (GEE) with a logit link and an exchangeable correlation matrix, to give population averaged estimates. Finally, as there was a sex imbalance among groups, we conducted a sensitivity analysis adjusting for sex.
3 Results
A total of 60 patients (12 males and 48 females) were recruited into this study and randomly assigned into 3 treatment groups. Baseline characteristics of each treatment group are shown in Table 1. The age ranged from 18 to 84 years (mean 34.4 ± 13.2 years). Most had medication failure (methimazole in 52 patients and propylthiouracil in 7 patients); one patient had never taken antithyroid drugs due to a drug allergy. The average duration of hyperthyroid therapy before I-131 ablation was 12 months. Thyroid gland size ranged from 50.1 to 288.2 grams (mean 96.2 ± 42.3 grams). The median of 4 to 24 hours thyroid uptake ratio was 1.07.
The median I-131 treatment dose in group A was 351.5 MBq or 9.5 mCi (range 203.5–1,924 MBq or 5.5–52.0 mCi), group B was 610.5 MBq or 16.5 mCi (range 370–1,202.5 MBq or 10.0–32.5 mCi) and group C was 925 MBq or 25.0 mCi (range 444–1,813 MBq or 12.0–49.0 mCi). According to Regulatory Guide 8.39 of the Nuclear Regulatory Commission (NRC) of the United States, an assigned dose of I-131 as outpatient treatment should be limited to 1,221 MBq (33 mCi). Therefore, 4 patients where the calculated dose of I-131 exceeded this level (1 patient with 1,924 MBq (52 mCi) in group A and 3 patients with 1,369 MBq (37.0 mCi), 1,535,5 MBq (41.5 mCi) and 1,813 MBq (49.0 mCi) in group C) were treated by splitting the dose over 2 consecutive days (The first day treated with 1,110 MBq (30.0 mCi) and the remaining dose given on the second day).
During follow-up, 6 patients received a second dose of I-131 due to no or minimal response to the first dose (1 in group A, 3 in group B and 2 in group C). Of these, 3 patients (1 in group A and 2 in group B) were cured after a second dose of treatment, but the remaining still had hyperthyroidism. One patient in Group C received a third dose of I-131 treatment and still had hyperthyroidism until 12 months. All of these patients were classified as cure failures over all follow-up in both ITT and available data analyses.
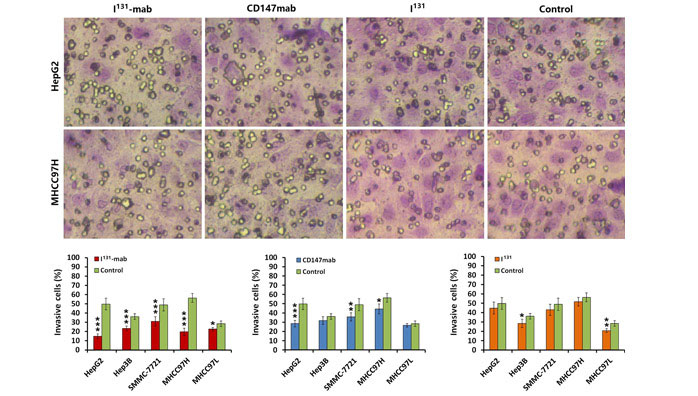
One patient in group A did not attend a 9-month follow-up visit; In group C, there were 1 patient, 3 patients, 2 patients and 1 patient who failed to attend their follow-up visits at 3, 6, 9, and 12 months, respectively. Tables 2 and 3 show the number of patients (%) cured in each group at each study week in the ITT and available data population. Figure 1 shows cure percentage at each follow up visit, by treatment group, in the ITT population. A higher proportion of patients were cured in group B and C than group A at all time points.
The primary endpoint analysis, which was the difference in cure percentage at 12 months, is shown in Table 4. A higher percentage of patients in group C were cured at 12 months compared to group A. The difference in percentage was 35 (95%CI 7.0–66.8)%; P = .02. The result was comparable in magnitude and statistical significance in the available data analysis. There were no differences in the cure proportions at 12 months in group B versus group A or group B versus group C in ITT or available data analyses.
As a secondary endpoint, we analysed the odds of cure in groups B and C versus group A as a reference (Table 5). The data were presented in both unadjusted and adjusted for gender difference due to the imbalance in the number of males assigned to each treatment group.
Patients in group C had 3.09 times higher odds of being cured at all points over follow-up compared to group A after adjusting for sex. Patients in group B also had higher odds of 2.18 of cure over all follow-up visits compared to group A, although the difference was not significant. Sex was not significantly associated with the outcome, and adjustment for sex had only a small impact on the odds ratios.
There were 7 patients who had side effects after the treatments as shown in Table 6: 2 in group A, 4 in group B and 1 in group C.
4 Discussion
An additive effect of lithium on radioactive iodine for the treatment of hyperthyroid patients has shown conflicting results for cure in a meta-analysis.[15] In observational trials, the cure rate was significantly higher in the lithium with I-131 treatment groups. However, interventional trials have not shown any significant additive effect. This might be due to smaller amounts of I-131 given, and shorter duration of antithyroid drug cessation, in a large randomized control trial compared with smaller trials, thereby affecting the pooled effect size in the interventional trials analysis. Another possible explanation is that selection and other biases inherent in observational studies, have influenced the findings. Using lithium carbonate with 3.7 mBq/g thyroid of I-131 for the treatment of Graves’ disease patients with rapid turnover uptake is a standard practice at our institution. This is because LiCO3 is known to improve I-131 retention in the thyroid gland, and is thus suitable for hyperthyroid patients with rapid turnover uptake.[9] However, it was observed that even with this regimen, the cure rate was still unimpressive. This might be due to similarly low amount of I-131 to the large randomized controlled trial in the meta-analysis mentioned above.[6] Such amount of I-131 given to the rapid turnover Graves’ disease patients may not be enough to render cure even though LiCO3 is given. Thus, the role of LiCO3 is unclear for this amount level of I-131. Factors leading to treatment failure are thyroid volume greater than 50 mL and 4/24-hour uptake ratio 0.8 or greater.[16] All of the patients in our study had thyroid gland size ≥50 grams, and all had a 4/24-hour uptake ratio of ≥1, factors known to be associated with high failure rates. The usual regimen for LiCO3 treatment in our institution is prescribing LiCO3 after I-131 treatment. I-131 is given in the late morning, then the patient is instructed to take first pill of LiCO3 after lunch on the day of treatment. We chose this regimen because many of our patients are sent from other hospitals and it is not always convenient to start LiCO3 before I-131 treatment. Furthermore, evidence suggests that prescribing LiCO3 after I-131 treatment produces similarly good outcomes to the pretreatment regimen.[8,17] This may be due to the fact that the peak serum concentration of LiCO3 is reached 0.5–2 hours after ingestion.
The design of this study was different from previous studies in that we compared standard I-131 dose (3.7 MBq/g thyroid) plus LiCO3 with the other two groups that we designed to give higher I-131 doses. One group with slightly higher dose plus LiCO3 and another with even higher dose without LiCO3, hypothesizing we would see higher cure rates in the latter two groups. The cure rate of patients at 12 months in group C who received the highest dose of I-131 of 7.4 MBq/g thyroid without LiCO3, was significantly higher than those receiving 3.7 MBq/g plus LiCO3 (group A). This was in line with the study by de Jong et al[16] who reported more cures in those receiving 7.4 MBq/ml when compared with those receiving 3.7 MBq/ml, but without prescribing LiCO3. We found that although we added LiCO3 to the 3.7 MBq/g group, there was still a significantly higher percentage of cures in the 7.4 MBq/mL group. The rate of cure in group B at 3 to 6 months after I-131 treatment was equal to group C, but the rate decreased at later time points (Fig. 1). This resulted in the non-significant difference of cure rate in group B when compared to group A. Therefore the dose of 1.5 times standard dose of I-131 plus LiCO3 (group B) may not be adequate to render enough cure even though Pusuwan et al[18] showed treatment with 5.5 MBq/g led to more cures than 3.7 MBq/g (70% vs 52%). The cure rate of group B in our study, which was 60% at 1 year, is less than that of Pusuwan's study. This may be because all patients in our study were Graves’ disease patients with rapid turnover, which is known to have a high treatment failure rate.[3] The decrease in the group B cure rate at 9 months and 12 months is likely due to transient hypothyroid at 3 to 6 months post I-131 treatment.[19,20] The mechanism underlying transient hypothyrodism is still unclear. A number of possibilities have been suggested, including transient hypofunction of hypothalamic-pituitary axis, depletion of thyroidal iodine storage by pretreatment antithyroid drugs, immunogenic (a shift between TSH receptor blocking and stimulating antibodies), or transient hibernation.[20] This effect was also seen in group A with an almost parallel curve to group B, though the cure rate was higher in group B (Fig. 1). The effect of transient hypothyroid was less in group C, probably due to the more permanent damage to the thyroid cells when compared to the other 2 groups.
Although group C did not show a statistically significant difference in cures compared to group B, the high rate of side effects of LiCO3 in this study found in groups A and B (Table 6) cannot be ignored. The reported side effect and toxicities of lithium [21] encompass tremor, nausea, vomiting, and diarrhea which are common in early treatment phases. Thirst, excessive urination, and weight gain are, in contrast, commonly found after long-term treatment. Cognitive impairment, dermatological effects (acne and psoriasis) seem to be dose related. There are long term effects on renal, thyroid and parathyroid function. Other than these side effects, fatigue, irritability and palpitation were also reported.[22] Mild lithium toxicity includes weakness, tremor, mild ataxia, poor concentration and diarrhea. The more toxic effect results in vomiting, gross tremor, slurred speech, confusion and lethargy. Some of these toxicities overlap with lithium side effects. A large interventional trial showed that approximately 10% of patients receiving lithium experienced mild to moderate side effects.[6] In our study, thirst was likely caused by LiCO3. Nausea and fatigue could be caused by either I-131 or LiCO3, while rash was thought to be associated with LiCO3.[23] Sialadenitis that occurred in a patient who received 29.5 mCi of I-131 was obviously due to I-131 treatment.[24] Irritability, palpitations, sweating and auditory hallucinations experienced by a patient in group B was more likely to be caused by I-131 than LiCO3. This is because the half-life of LiCO3 is 18–24 hours, thus any symptoms occurred after 4 to 6 half-lives is less likely to be caused by lithium. Symptoms in this patient which occurred after 14 days of I-131 treatment, may be due to more thyroid hormone release into the blood stream after I-131 treatment. The symptoms of so-called thyrotoxic psychosis, as previously reported.[25]
From Table 1, all baseline characteristics are balanced due to the randomised nature of this study, except for a higher proportion of females in groups A and B versus group C. In a sensitivity analysis, we performed an adjusted analysis of our secondary endpoint corrected for sex, but there was no important impact on the result (Table 5). In an ITT population, group C had 2.85 times of odds of cure versus group A in nongender adjusted model and 3.09 times in sex-adjusted model. When analyzed using available data only, there was 3.22 and 3.62 times of odds of cure comparing group C and A in the nonadjusted and gender-adjusted model, respectively.
There were 4 cases (group A and group C) that the treatment was divided into two consecutive days due to the calculated I-131 dose of more than 1,221 MBq (33.0 mCi). Previous studies showed that the thyroid gland can still take up I-131 without a stunning effect, when the first and second doses of I-131 are given up to 48 hours apart. If the second dose I-131 is given after 72 hours, the ability to capture I-131 drops dramatically (a phenomenon known as thyroid stunning).[26,27] Based on these studies, 2 patients in group C who received 1,535.5 MBq (41.5 mCi) and 1,813 MBq (49.0 mCi) were found to have cure at 12 months. Another 2 patients, 1 in group A (1,924 MBq or 52.0 mCi) and 1 in group C (1,369 MBq or 37.0 mCi), were not cured.
There are a number of limitations of this study. First, our study was small with limited power to discern if there was a difference in efficacy between groups B and C, and therefore we recommend additional larger studies examine this issue. Second, some side effects of I-131 or LiCO3 can also be caused by other health conditions, for example nausea/vomiting can be due to gastritis or other underlying gastrointestinal conditions, and auditory hallucination can be caused by psychosis. To mitigate the risk of wrongly attributing these adverse events to a study drug, we checked that the symptoms were new and only occurred after study drug administration.
In conclusion, treatment of rapid turnover Graves’ disease patients with high dose (7.4 MBq/g or 200 microCi/g) I-131 has high cure rate at 12 months (80%) with lower side effects when compared to other groups. It provides approximately 3 times higher odds of cure over follow-up than those using 3.7 MBq/g or 100 microCi/g I-131 plus LiCO3. We thus recommend this treatment regimen in Graves’ disease patients with rapid turnover uptake.
The information comes from:
https://journals.lww.com/md-journal/Fulltext/2019/05100/Finding_the_best_effective_way_of_treatment_for.83.aspx